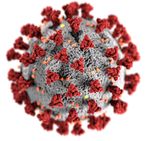
COVID-19 coronavirus and cancer
The intent of this page is to gather information relevant to COVID-19, the disease caused by SARS-CoV-2 virus. If you are viewing this page on a cellphone or tablet, consider loading up the desktop version of this page so that a table of contents for the page is displayed for you.
This page is a gathering point for many different topics related to COVID-19. Some are cancer-specific, others are not. If you are a health care professional looking for clinical guidance, you may want to go directly to information for health care professionals, potential treatments, or to the testing sections. The literature on COVID-19 and cancer is just beginning to emerge; we will attempt to keep pace in the scientific evidence section.
Please contribute to this page, including correcting and deleting erroneous or outdated content. The content of this page as well as the pandemic are both evolving quickly, and we need help to keep the page as useful as possible! If you don't have an account, sign up here. If you've signed up but don't have editing privileges yet, email [email protected].
COVID-19 and Cancer Consortium (CCC19)
On March 17th, a registry was launched to capture information about US-based cancer patients who have been affected by COVID-19. Please check out the website with link to survey tool here.
Institutions and organizations participating in the consortium include:
- Aurora Health
- City of Hope
- Cleveland Clinic
- Dana-Farber Cancer Institute
- Duke University
- Emory University
- Intermountain Health
- Johns Hopkins University
- Mayo Clinic
- Mount Sinai/Tisch Cancer Institute
- NCI Bethesda
- Northwestern University Lurie Cancer Center
- The Ohio State University
- Stanford University
- University of California, Davis
- University of California, San Diego
- University of Connecticut
- University of Miami/Sylvester Comprehensive Cancer Center
- University of North Carolina
- University of Washington/Seattle Cancer Care Alliance/Fred Hutch
- Vanderbilt University Medical Center
- Washington University in St. Louis
- West Cancer Center
General information relevant to cancer patients
- Cancer.gov: Coronavirus: What People with Cancer Should Know (official website of the National Cancer Institute)
- Cancer.net: Coronavirus 2019: What People With Cancer Need to Know
- Fred Hutch: What cancer patients need to know
- What Cancer Patients, Survivors, and Caregivers Need to Know about the Coronavirus
- What Cancer Patients Need to Know about Coronavirus COVID-19 (Salud America!)
- UK CLL forum guidance on COVID-19 for patients with CLL (Twitter @Ukcll, 3/12/2020)
Information for healthcare professionals
| back to top |
Oncology
Guidance for Treatment of Patients with Cancer and Containment of COVID-19: Experiences from Italy
Curigliano G, ASCO Daily News 3/17/20
- Cancer patients stratified into two groups
- (A) Patients who completed treatment or whose disease is under control
- (B) Patient undergoing treatment (neoadjuvant or adjuvant curative treatment or treatment for metastatic disease)
- For patients receiving active treatment (B), living in epidemic zones or not, identified specific pathways in order to guarantee timing of treatment with curative intent and, when possible, also for patients with metastatic disease
- Four "Hub Cancer Centers" have been designated in the Lombardy area where cancer can be transferred to receive surgery or active chemotherapy/radiotherapy, biologic therapy, and immunotherapy
- Hub Center should guarantee an appropriate diagnostic-therapeutic pathway that reduces the risk of COVID-19 infection for all patients
- Hub Center should establish checkpoint areas screening for early detection of potential infectious persons with protocols for testing and transferring to COVID-19 hospitals if warranted
| Setting | Strategy | Measures |
|---|---|---|
| Patients "off treatment" |
|
|
| Patients with early stage cancer in a curative setting (neoadjuvant treatment, surgery, and adjuvant treatment) |
|
|
| Patients with metastatic disease |
|
|
Guidance for immune checkpoint inhibitors and COVID-19
Courtesy of Dr. Douglas Johnson (VUMC)
- The effects of immune checkpoint inhibitors (ICI), including anti-PD-1, anti-PD-L1, and anti-CTLA-4 agents on COVID-19 infections have not been determined.
- While these agents do not produce an immunocompromised state (in contrast to cytotoxic chemotherapy), there is theoretical concern that they could potentiate pulmonary inflammation induced by the virus.
- Patients who urgently need therapy should initiate ICIs; delaying therapy until after the pandemic could be considered in patients without an urgent indication to start therapy (e.g. stage III melanoma patient to receive adjuvant therapy, indolent/slowly progressive renal cell carcinoma).
- In patients who develop a dry cough while receiving ICI, both ICI-pneumonitis and COVID-19 infection (as well as other infectious etiologies) should be considered. Viral testing should be performed to rule out COVID-19 infection. The presence of a fever may suggest a viral (or bacterial) origin, while lack of a fever may suggest ICI-pneumonitis. However, radiographic presentations and symptoms may overlap.
- All patients receiving ICI with presumed pneumonitis should be tested for COVID-19 and isolated until testing is negative. If COVID positive, consider adding hydroxychloroquine 400mg q12h on day 1, then 200mg daily days 2-5 per institutional guidelines. If no response in 48-72 hours, consider tocilizumab.
- In patients diagnosed with COVID-19, we would recommend postponing resumption or initiation of ICI therapy for approximately 2 weeks after clinical resolution of symptoms or after first negative viral test.
- In critically ill patients who are receiving ICI and are diagnosed with COVID-19, steroids (e.g. prednisone 1mg/kg) could be considered although the role of steroids is highly questionable (given their potentially detrimental effects on viral clearance in other coronavirus infections). (? Role of tocilizumab -studies ongoing?)
Guidance for immune cellular therapy
- Fred Hutch recommendations
- The IMTX program will continue to offer commercial CAR T treatments and enroll patients in cellular immunotherapy clinical trials where there is demonstrated benefit.
- Decisions on other cellular immunotherapy clinical trials will be made on a case by case basis and the IMTX program may delay enrollment to clinical trials with significant inpatient resource utilization.
Guidance for lung cancer patients
Courtesy of Nagla Abdel Karim, MD, PhD (Professor of Medicine, Augusta University-Georgia Cancer Center) in discussion with colleagues who are oncologists in Milan-Italy:
- Newly diagnosed patients especially of small cell lung cancer; neoadjuvant, adjuvant and metastatic disease with appropriate performance status remain a priority to treat and receive growth factors support with myelosuppresive therapies.
- Clinical trials patients remain of priority too, however follow up or lab based visits; consider tele-oncology to prevent too many visits that might risk patients’ during the epidemic.
- Maintenance patients can be off treatment for 2 months (break of therapy if possible as long as the disease is stable).
- Patients admitted with severe neutropenia should not be discharged with the severe neutropenia, but remain until their counts recover.
- Follow up patients should either follow through tele-oncology or postpone clinic visit for 3 months (in Italy they were postponed for 3 months, but here, I would like to propose a tele-oncology format).
Guidance for transplant
- American Society for Transplantation and Cellular Therapy (ASTCT) Interim guidelines for COVID-19 management in hematopoetic cell transplant and cellular therapy patients
- Mayo Clinic recommendations (Vincent Rajkumar's original Twitter thread):
- We recommend DELAY the whole transplant process (collection, & storage) for all newly diagnosed patients until the corona epidemic is over.
- If myeloma patients are already on transplant schedule, we recommend offer to delay the whole process (collection and storage) until the corona epidemic is over. If patients are already on site, collect cells but delay the transplant.
- For patients who need the transplant for progressive disease, or very high risk disease and expected early relapse and cannot wait to delay, proceed with transplant.
- Fred Hutch recommendations
| Transplant type | Delay | Consider delay | Proceed with transplant |
|---|---|---|---|
| Allogeneic | 1. Intermediate-risk AML in MRD-negative CR1 tolerating consolidation 2. ALL in MRD-negative CR1 tolerating maintenance/consolidation 3. MDS without excess blasts (RA, SLD, etc) tolerating transfusions 4. Myelofibrosis/MPN/CMML with low blast count without evidence of rapid disease progression, tolerating transfusions |
1. MDS-EB 2. CMML-1 and 2 |
1. High-risk AML in CR1 2. AML and ALL beyond CR1 3. Secondary AML (evolved from MDS, MPN, etc) |
| Autologous | 1. Multiple myeloma (consider stem cell collection only depending on extent of prior treatment) 2. Low-grade lymphoma (Follicular lymphoma, Mantle cell lymphoma, etc) 3. Autoimmune diseases (MS, scleroderma, etc) |
Aggressive lymphomas (DLBCL, etc) |
Podcasts
Critical care/ICU
| back to top |
- GiViTI 3/10/2020 COVID-19 meeting about intensive care patients - patient characteristics and management recommendations (Posted at: criticalcarenorthampton.com link to original document)
- Critical care resources for non-ICU clinicians (propofology.com)
- Royal London Hospital COVID Intubation SOP (Twitter @DrJEMcK, 3/14/2020; link to Powerpoint file)
- COVID-19 intubation tutorial (Youtube)
Radiology
- Example, CT chest with fibrosis/ARDS (Twitter @danortizmd 3/15/2020)
- COVID-19 severe ARDS (Twitter @curijoey 3/14/2020)
PPE (personal protective equipment)
- Improvised reusable elastomeric respirator, Surgical Innovation Fellowship, Boston Children's Hospital (Youtube)
- "Addressing COVID-19 Face Mask Shortages" (Stanford) - with statistics about performance of N95 masks' filtration efficiency after disinfection
- 3M technical bulletin 3/20/2020 recommended against "Disinfection of Filtering Facepiece Respirators"
- Microwave generated steam, ultraviolet irradiation, and moist heat damaged components of respirators such as elastic straps and plastic surrounding metal nose clips and staples
Other
| back to top |
- DEA COVID-19 Information Page
- ABIM Coronavirus Updates
- AMA COVID-19 FAQ
- University of Washington COVID-19 Resource Site
- COVID-19 infographic about Italian experience by Twitter @FOAMecmo
- IDSA COVID-19 resource center
- Johns Hopkins Coronavirus COVID-19 (SARS-2-CoV) management information
- Proposed initial diagnostic and management workflow for potential COVID-19 cases given limited testing capacity (Twitter @srrezaie, 3/8/2020)
- MGH Grand Rounds Video: A Coordinated, Boston-wide Response to COVID-19 (3/12/2020)
- Dr. Sachin Shah at UCSF COVID-19 references
- Coronavirus tech handbook (shared Google Doc of clinical care)
- Notes (3/8/2020) from infectious disease physician Martha L. Blum, MD, PhD from Infectious Disease Association of California (IDAC) Northern California Winter Symposium on Saturday 3/7/2020:
- In attendance were physicians from Santa Clara, San Francisco & Orange Counties who had all seen and cared for COVID-19 patients, both returning travelers and community-acquired cases. Also present was the Chief of ID for Providence, who has 2 affected Seattle hospitals. Erin Epson, CDPH director of Hospital Acquired Infections, was also there to give updates on how CDPH and CDC are handling exposed health care workers, among other things. Below are some of the key take-aways from their experiences.
- The most common presentation was 1 week prodrome of myaglias, malaise, cough, low grade fevers gradually leading to more severe trouble breathing in the 2nd week of illness. It is an average of 8 days to development of dyspnea and average 9 days to pneumonia/pneumonitis. It is not like Influenza, which has a classically sudden onset. Fever was not very prominent in several cases. The most consistently present lab finding was lymphopenia (with either leukocytosis or leukopenia). The most consistent radiographic finding was bilateral interstitial/ground glass infiltrates. Aside from that, the other markers (CRP, PCT) were not as consistent. Co-infection rate with other respiratory viruses like Influenza or RSV is <=2%, interpret that to mean if you have a positive test for another respiratory virus, then you do not test for COVID-19. This is based on large dataset from China. So far, there have been very few concurrent or subsequent bacterial infections, unlike Influenza where secondary bacterial infections are common and a large source of additional morbidity and mortality.
- Patients with underlying cardiopulmonary disease seem to progress with variable rates to ARDS and acute respiratory failure requiring BiPAP then intubation. There may be a component of cardiomyopathy from direct viral infection as Intubation is considered “source control” equal to patient wearing a mask, greatly diminishing transmission risk. BiPAP is the opposite, and is an aerosol generating procedure and would require all going into the room to wear PAPRs.
- To date, patients with severe disease are most all (excepting those whose families didn’t sign consent) getting Remdesivir from Gilead through compassionate use. However, the expectation is that avenue for getting the drug will likely close shortly. It will be expected that patients would have to enroll in either Gilead’s RCT (5 vs 10 days of Remdesivir) or the NIH’s “Adaptive” RCT (Remdesivir vs. Placebo). Others have tried Kaletra, but didn’t seem to be much benefit.
- If our local MCHD lab ran out of test kits we could use Quest labs to test. Their test is 24-48 hour turn-around-time. Both Quest and ordering physician would be required to notify Public Health immediately with any positive results. Ordering physician would be responsible for coordinating with the Health Department regarding isolation. Presumably, this would only affect inpatients though since we have decided not to collect specimens ordered by outpatient physicians.
- At facilities that had significant numbers of exposed healthcare workers they did allow those with low and moderate risk exposures to return to work well before 14 days. Only HCW with highest risk exposures were excluded for almost the full 14 days (I think 9 days). After return to work, all wore surgical masks while at work until the 14 days period expired. All had temp checks and interview with employee health prior to start of work, also only until the end of the 14 days. Obviously, only asymptomatic individuals were allowed back.
- Symptom onset is between 2-9 days post-exposure with median of 5 days. This is from a very large Chinese cohort. Patients can shed RNA from 1-4 weeks after symptom resolution, but it is unknown if the presence of RNA equals presence of infectious virus. For now, COVID-19 patients are “cleared” of isolation once they have 2 consecutive negative RNA tests collected >24 hours apart.
- All suggested ramping up alternatives to face-to-face visits, tetemedicine, “car visits”, telephone consultation hotlines. Sutter and other larger hospital systems are using a variety of alternative respiratory triage at the Emergency Departments. Health Departments (CDPH and OCHD) state the Airborne Infection Isolation Room (AIIR) is the least important of all the suggested measures to reduce exposure. Contact and droplet isolation in a regular room is likely to be just as effective. One heavily affected hospital in San Jose area is placing all “undifferentiated pneumonia” patients not meeting criteria for COVID testing in contact+droplet isolation for 2-3 days while seeing how they respond to empiric treatment and awaiting additional results.
- Feel free to share. All PUIs in Monterey Country so far have been negative. Martha L. Blum, MD, PhD
Potential treatments
Coming soon, please help flesh this out!
Colchicine
Hydroxychloroquine
- Gautret et al. Hydroxychloroquine and azithromycin as a treatment of COVID‐19: results of an open‐label non‐randomized clinical trial. International Journal of Antimicrobial Agents – In Press 17 March 2020. Link to original article.
- Inclusion Criteria
- Age >12 years
- PCR-documented SARS-CoV-2 carriage in nasopharyngeal sample at admission
- Treatment
- Hydroxycholorquine 200mg PO TID x 10 days
- Clinician option to add Azithromycin 500mg PO on day 1 followed by 250mg PO daily on days 2-5
- Results
- 20 patients treated with hydroxychloroquine had a significantly higher rate of viral nasopharyngeal clearance (PCR negative) at 6 days post-treatment than control (70% vs 12.5%, p= 0.001)
- Subset of 6 patients treated with hydroxycholorquine plus azithromycin had 100% viral nasophranygeal clearance at 6 days compared with hydroxychloroquine alone (57.1%) and control (12.5%)
- Inclusion Criteria
- Cao et al. A Trial of Lopinavir–Ritonavir in Adults Hospitalized with Severe Covid-19. Link to original article. Pubmed.
- Inclusion Criteria
- >18 years old
- RT-PCR confirmed SAR-CoV-2 in a respiratory tract sample
- Pneumonia confirmed by chest imaging
- O2 < 94% on RA or PaO2:FiO2 < 300 mmHg
- Treatment
- Lopinavir-Ritonavir 400mg - 100mg PO BID
- Results
- No difference in time to clinical improvement between Lopinavir-Ritonavir (99 pts) vs standard treatment alone (100 pts) (16 days vs 16 days [HR 1.31, 95% CI 0.95-1.85])
- No difference in time to clinical deterioration between Lopinavir-Ritonavir (99 pts) vs standard treatment alone (100 pts) (HR 1.01, 95% CI 0.76 - 1.34)
- Inclusion Criteria
Remdesivir
- Holshue et al. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med 2020; 382:929-936. Link to original article. Pubmed.
- Case report of 1 patient with clinical improvement after Remdesivir
Tocilizumab
- Xu et al. Effective Treatment of Severe COVID-19 Patients with Tocilizumab. ChinaXiv:202003.00026. Link to original article.
- Inclusion Criteria
- Severe or critical pneumonia
- Severe defined as any of the following: RR>30, SpO2<93% on RA, or PaO2/FiO2 < 300 mmHG
- Critical defined as any of the following: respiratory failure which required mechanical ventilation, shock, or need to be admitted to ICU combined with other organ failure
- RT-PCR confirmed SARS-CoV-2 by throat swab
- Severe or critical pneumonia
- Treatment
- Tocilizumab 400mg IV x1
- Results
- 20 patients treated with tocilizumab all had resolution of fevers within 1 day of treatment, 15 (75%) lowered their oxygen requirements, 19 (90.5%) clinically improved and were discharged from hospital
- Inclusion Criteria
Scientific Evidence on COVID-19 Occurrence in Cancer Patients
| back to top |
General cancer
- Liang W, Guan W, Chen R, Wang W, Li J, Xu K, Li C, Ai Q, Lu W, Liang H, Li S, He J. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020 Mar;21(3):335-337. Epub 2020 Feb 14. link to original article PubMed.
- As of Jan 31, 2020, authors collected 2007 cases (417 cases were subsequently excluded due to insufficient records) from 575 hospitals (appendix pp 4–9 for a full list) in 31 provincial administrative regions. All cases were diagnosed with laboratory-confirmed COVID-19 acute respiratory disease and were admitted to hospital. Only 18 (1%; 95% CI 0·61–1·65) of 1590 COVID-19 cases had a history of cancer, which was higher when compared with the incidence of cancer in the overall Chinese population (0·29%).
- Among cancers identified, lung cancer was the most frequent type (five [28%] of 18 patients).
- Compared with patients without cancer, patients with cancer were older (63·1 vs. 48.7 years), more likely to have a history of smoking (22% vs. 7%), and more severe baseline CT manifestation (94% v.s. 71%), but had no significant differences in sex, other baseline symptoms, other comorbidities, or baseline severity of x-ray.
- Patients with cancer were observed to have a higher risk of severe events (a composite endpoint defined as the percentage of patients being admitted to the intensive care unit requiring invasive ventilation, or death) compared with patients without cancer (seven [39%] of 18 patients vs 124 [8%] of 1572 patients; Fisher’s exact p=0·0003).
- Patients who underwent chemotherapy or surgery in the past month had a numerically higher risk (three [75%] of four patients) of clinically severe events than did those not receiving chemotherapy or surgery (six [43%] of fourteen patients)
- Two Editorials Addressed to this:
- Wang H, Zhang L. Risk of COVID-19 for patients with cancer. Lancet Oncol. 2020 Mar 3:S1470-2045(20)30149-2. link to original article PubMed
- Of the 16 patients who had known treatment status, only four had undergone surgery or chemotherapy within the previous month; 12 had recovered from initial cancer treatments (eg, surgery or chemotherapy) and had no obvious immunosuppression. Hence, the correlation between the COVID-19 infections and cancers in the 12 cancer survivors was questionable.
- Liang et al. reported patients with cancer had worse outcomes from COVID-19, but the median age of these patients (63·1 years) was significantly higher than for those without cancer (48·7 years), suggesting that older age is associated with worse COVID-19 outcomes.
- Xia Y, Jin R, Zhao J, Li W, Shen H. Risk of COVID-19 for cancer patients. Lancet Oncol. 2020 Mar 3:S1470-2045(20)30150-9. link to original article PubMed
- Instead of the showing a higher percentage of COVID-19 patients having cancer, the incidence of COVID-19 in patients with cancer would be more informative in assessing whether or not patients with cancer have an increased risk of COVID-19.
- Authors also criticized the limitations of: small sample size, large amount of heterogeneity, various cancer types with different biological behaviours variable disease courses (from 0–16 years), and diverse treatment strategies and felt that the cohort was not ideally representative of the whole population with cancer.
- The significant smoking history in the 18 patients with cancer could be a possible confounder given that data has shown that tobacco use significantly increases the gene expression of angiotensin converting enzyme 2 (the binding receptor for severe acute respiratory syndrome coronavirus 2) which could explain the elevated susceptibility to COVID-19 in smokers. The association of smoking with COPD is also another independent risk factor in COVID-19 cases.
- Wang H, Zhang L. Risk of COVID-19 for patients with cancer. Lancet Oncol. 2020 Mar 3:S1470-2045(20)30149-2. link to original article PubMed
- Yu et al. [Not Peer-Reviewed]: https://doi.org/10.1101/2020.02.22.20025320doi:
- Between Dec 30, 2019 to Feb, 17 2020, studied a total of 1,524 cancer patients managed at Zhongnan hospital of Wuhan University
- Among them, the three commonest cancer diagnoses were gastrointestinal (N = 394,35.9%), thoracic (N = 326, 21.4%), and head and neck cancers (N = 204, 13.4%).
- The authors estimated that the infection rate of SARS-CoV-2 in cancer patients from single institution at 0.79% (95% CI = 0.3–1.2) which was higher than the cumulative incidence of all diagnosed COVID-19 cases that was reported in the city of Wuhan over the same time-period (0.37%, 41,152/11,081,000 cases, data cutoff on Feb 17, 2020).
- Thus, the authors found that cancer patients had an estimated 2-fold increased risk of COVID-19 than the general population.
- Interestingly, only five of these patients were ongoing treatment at the time of contracting the virus, suggesting that hospital visitation was the likely factor contributing to the elevated incidence in cancer patients.
- Moreover, the observed the incidence of severe COVID-19 was not higher than in the general population (Note: This is contradictory to the finding of Liang et al.)
- Zhang H, Huang Y, Xie C. The Treatment and Outcome of a Lung Cancer Patient Infected with SARS-CoV-2. Journal of Thoracic Oncology (2020). Link to original article.
- Case report of 57 year-old Chinese male with EGFR+ advanced lung adenocarcinoma on osimertinib and undergoing radiation therapy one month prior to developing COVID-19. He was treated with Lopinavir-Ritonavir with clinical improvement and clearance of serial RT-PCR's. He continued his osimertinib throughout COVID-19 clinical course with repeat chest imaging after discharge showing stable lung cancer lesions.
Lung cancer
| back to top |
- Lung Cancer Study Group, Chinese Thoracic Society, Chinese Medical Association; Chinese Respiratory Oncology Collaboration. [Expert recommendations on the management of patients with advanced non-small cell lung cancer during epidemic of COVID-19 (Trial version)]. Zhonghua Jie He He Hu Xi Za Zhi. 2020 Mar 3;43(0):E031. Chinese. link to original article PubMed
- A guideline for the optimal management of patients with advanced lung cancer was proposed to distinguish the symptoms of COVID-19 and the side effects of antitumor drugs.
- A questionnaire survey was conducted on the lung cancer group of the Chinese Thoracic Society, Chinese Medical Association; the lung cancer group of the Chinese Society of Clinical Oncology Youth Committee; and the Chinese Respiratory Oncology Collaboration.
- Based on the 321 validated questionnaire survey results the following recommendations were made:
- Patients with advanced NSCLC should be treated as outpatients if possible at the nearest medical center
- Patients who need to be hospitalized for antitumor treatment should be tested negative for COVID-19 infection
- Close attention should be paid to identification of COVID-19-related symptoms and adverse reactions caused by the malignancy or antitumor treatments.
- Stronger personal protection should be made for advanced NSCLC patients
- An intentional postponing of antitumor treatment should be considered according to patient performance status.
- Treatment strategies should be made according to different types of advanced NSCLC patients and efficacy and toxicity of drugs.
Reports of medical center experiences
| back to top |
Canada
- "Here in Vancouver I’ve seen 5 COVID19 cases; 2 are nurses without travel history or sick contacts. We have only had to intubate 1 patient in the whole province. Already extubated." (Twitter @jeremyfaust 3/14/2020)
Italy
- The Treatment of Patients With Cancer and Containment of COVID-19: Experiences From Italy ASCO Daily News, 3/17/2020
- "The current situation is difficult to imagine and numbers do not explain things at all. Our hospitals are overwhelmed by Covid-19, they are running 200% capacity" (Twitter @jasonvanschoor, 3/9/2020)
- "Cases are multiplying, we arrive at a rate of 15-20 admissions per day all for the same reason. The results of the swabs now come one after the other: positive, positive, positive. Suddenly the E.R. is collapsing." - ICU physician in Bergamo, Dr. Daniele Macchini. (Twitter @silviast9 3/9/2020 interpreted translation from original document, Con le nostre azioni influenziamo la vita e la morte di molte persone)
- "Very aggressive disease, many young and fit people severely ill, some colleagues too. We're turning ORs into ICUs to increase positive pressure beds with respirators" (Twitter @EvaristoCroce, 3/9/2020)
- "Today, some hospitals are so overwhelmed that they simply cannot treat every patient. They are starting to do wartime triage." (Twitter @Yascha_Mounk, 3/11/2020 interpreted translation from original document, RACCOMANDAZIONI DI ETICA CLINICA PER L’AMMISSIONE A TRATTAMENTI INTENSIVI E PER LA LORO SOSPENSIONE)
- "We stop intubating people over 60. We leave them die. 30 per cent of patient are 30-60 years old. We have no more ventilators for all patients. 600 intubated in milan.... We are ready to sacrifice our lives to stop it.... There are no more surgeons or dermatologist--only doctors--all together to stop it." (Twitter @Strosterud 3/12/2020)
- "He had to let 3 people die that day, nurses crying because they see people dying in front of them and can't do anything aside from offering some oxygen." (Reddit u/goddessofthebitches 3/12/2020)
- Critical Care Utilization for the COVID-19 Outbreak in Lombardy, Italy - Early Experience and Forecast During an Emergency Response, Giacomo Grasselli, MD; Antonio Pesenti, MD; Maurizio Cecconi, MD3, JAMA 3/13/2020 -- Companion 3/13/2020 JAMA Youtube video interview with Maurizio Cecconi MD "If you don't take down the transmission of the virus, then the capacity of your system will be overwhelmed." - 29:27
- “Single isolation was only for our detection period. As soon as a #COVID19 test is positive, transfer the patient to cohort isolation. At some point your negative pressure rooms are full – and you cannot isolate anyone else" “We are in a war zone here. In our 1000 bed hospital we closed up wards & programs, all outpatient clinics & built up cohort areas. Now, we have 400 #COVID19 patients. 56 intubated, 2 ECMO, 2 ECCOR, 12 on NIV, 80 CPAP on wards” (Twitter @PedsIntensiva 3/14/2020)
- "As many as 5 to 10 percent of the severe cases and of deaths are actually among the healthcare personnel.... We forget to eat, we forget to drink, and we keep on working.... The worse is somebody dying in the isolated ward asking for the wife, the husband, for the last hours of their life and having no chance to have anybody around and dying on their own." Italian doctors interviewed by New York Times (Youtube 3/23/2020)
South Korea
- "Emphasis was placed on transparency, rapidly available and accurate information. Transparency is essential to ensure active participation from citizens." (Twitter @HannahNamMD, 3/11/2020), English Youtube video of South Korea 3/9/2020 briefing about COVID-19)
Spain
- "Spreading there very fast with young people in ICUs now and doctors getting infected" (Twitter @david raben 3/14/2020)
- Difficult decisions made to transition care to younger patients, in Spanish (Twitter @WellingMichael 3/21/2020)
United Kingdom
"Today in our trust we are closing CCU to modify it to have ventilators for COVID patients. 7 extra ITU beds at Western Sussex NHS." (Twitter @kristelly79 3/13/2020)
United States
| back to top |
Boston
- "We are rapidly shutting down routine care. We have canceled all planned follow-ups with patients with diabetes and heart failure at this point because we have to preserve that personal protective equipment." (Dr. Daniel Horn with Franklin Foer, The Atlantic 3/16/2020)
New York
- "We already have #COVID19 cases. The # increases EVERY day. If they keep going at this rate, our system will be overwhelmed. We won’t have the space, personnel or supplies to provide the best care to our #coronavirus AND our regular patients." (Twitter @Craig_A_Spencer 3/15/2020)
- "8 COVID patients with ARDS in ICU and half were severe. My team proned 3 of the severe ARDS with good response to PEEP and proning." (Twitter @MichelleNgGong 3/15/2020)
- "We are seeing sudden deterioration with arrhythmias and cardiac arrest. Can't tell yet if it is viral myocarditis and still not enough sample size for me to call it an association but it is notable to me." (Twitter @MichelleNgGong 3/15/2020)
- "They’re dangerously short on supplies. Her entire floor, roughly 30 people, was given two boxes of masks for a total of 100. The hospital has told them they need to make them last for at least two weeks. That’s roughly 3.33 masks per health worker" (Twitter @evansiegfried 3/18/2020)
- "Our most senior clinicians are saying what is obvious to anyone on the front lines right now: COVID-19 is unprecedented and dire." (Facebook Colleen Farrell, MD 3/20/2020)
- "Spoke to physician friends in NYC. Situation quickly deteriorating... multiple hospital floors designated as COVID, ICU quickly filling, Jacobs Javits Center converted to 1000 bed COVID hospital, military deployed, Navy Hospital Ship to NYC Harbor" (Twitter @BioBreakout 3/21/2020)
- "The difference in the ER from last week to this week is stark. Last Sunday: a few #COVIDー19 + patients mixed w/ the chest pains, abdominal pains, etc. Today: overwhelming majority are #COVIDー19 suspected/confirmed. Very little of anything else." (Twitter @Craig_A_Spencer 3/22/2020)
- "Finally home after 13 hours in the ER. Today >90% of my patients were confirmed or likely #COVID19. Many really sick, some in their 30s like me. The sirens on otherwise empty NYC streets are unending & haunting." (Twitter @Craig_A_Spencer 3/22/2020)
- "The stress is being felt across entire hospitals and health systems. Many people are working longer hours, people are working extra shifts, and people are being asked to step out of their normal roles and contribute in other ways." (Dr. Caldwell at NYU via Twitter @evankirstel 3/22/2020)
San Francisco
- "We continue to face inadequate COVID-19 testing capacity. This is a national crisis.... At SF General Hospital, we’ve created and operationalized a quick low radiation dose chest CT that takes very little time, and has been very useful in helping us evaluate and risk stratify patients." (Twitter @VivekJainMD 3/12/2020)
- "Shortages real: have enough PPE now but may run out soon. Testing: doing ~100/d now, but big shortage of reagent & swabs may force cuts. Beds, ICUs, vents OK for now but seeking more if we need, including at other SF hospitals. Blood shortage looming" (Twitter @Bob_Wachter 3/18/2020)
- "Very mild uptick in volume today: 8 patients in hospital with confirmed #COVID19 (2 in ICU), 18 w/ tests pending. Other COVID+ patients doing OK as outpatients.... PPE shortage dire–limiting MDs seeing pts to one (& subbing inpt televisits), no pt visitors, reusing PPE if safe. A tension all over: areas in which evidence-based guidelines say surgical mask/eye protect good enough, but some feel more secure w/ N95." (Twitter @Bob_Wachter 3/19/2020)
- "Shortages: still big problems w/ swabs, gowns, masks. Many(!) offers of donations–we're organizing to manage. Testing growing; amazing that swabs will be hurdle c) Rule changes: interstate #Telehealth visits now OK; MDs/RNs can work if back from Level 3 country & no sxs" (Twitter @Bob_Wachter 3/20/2020)
- "Still not seeing NY-like surge: such sad stories there, system nearly overwhelmed. Our PPE stable, though tenuous; grateful for donations. Some hope on swab front." (Twitter @Bob_Wachter 3/22/2020)
- Interview with Dr. Bob Wachter with Dr. Armond Esmaili, Medical Director of COVID isolation floor at UCSF (Youtube 3/23/2020)
- "Still just 10 Covid pts @ucsfhospitals...Testing @ucsf now ramped up to ~400/day. Limiting factor was the special swabs... We just received ~4000 of them from federal emergency stockpile, which relieves that bottleneck, at least for now. We’re still triaging testing; not testing asymptomatic people for now. With each day w/o big surge, we struggle re: elective surgeries/transfers. Currently doing ~none, but ? when are we safe to open up? One 1 hand, major need/backlog. On other, must save capacity, esp. after hearing how fast @nyphospital was overrun w/ Covid pts." (Twitter @Bob_Wachter 3/23/2020)
Seattle
- "We are seeing pts who are young (20s), fit, no comorbidities, critically ill. It does happen.... Currently, all of ICU is for critically ill COVIDs, all of floor medsurg for stable COVIDs and EOL care, half of PCU, half of ER. New resp-sx pts in Pulmonary Clinic as offshoot" (Twitter @Chenbariatrics1 3/13/2020)
- March 10,2020 “This is from a front-line ICU physician in a Seattle hospital This is his personal account:
- we have 21 pts and 11 deaths since 2/28.
- we are seeing pts who are young (20s), fit, no comorbidities, critically ill. It does happen.
- US has been past containment since January
- Currently, all of ICU is for critically ill COVIDs, all of floor medsurg for stable COVIDs and EOL care, half of PCU, half of ER. New resp-sx pts in Pulmonary Clinic as offshoot
- CDC is no longer imposing home quarantine on providers who were wearing only droplet iso PPE when intubating, suctioning, bronching, and in one case doing neurosurgery. Expect when it comes to your place you may initially have staff home-quarantined.
- Plan for this NOW. Consider wearing airborne iso PPE for aerosol-generating procedures in ANY pt in whom you suspect COVID, just to prevent the mass quarantines.
- we ran out of N95s (please stop hoarding!) and are bleaching and re-using PAPRs, which is not the manufacturer's recommendation. Not surprised on N95s as we use mostly CAPRs anyway, but still.
- terminal cleans (inc UV light) for ER COVID rooms are taking forever Enviro Services is overwhelmed. Bad as pts are stuck coughing in the waiting room. Rec planning now for Enviro upstaffing, or having a plan for sick pts to wait in their cars (that is not legal here, sadly)
- CLINICAL INFO based on our cases and info from CDC conf call today with other COVID providers in US:
- the Chinese data on 80% mildly ill, 14% hospital-ill, 6-8% critically ill are generally on the mark.
- Data very skewed by late and very limited testing, and the number of our elderly pts going to comfort care.
- being young & healthy (zero medical problems) does not rule out becoming vented or dead
- prob the time course to developing significant lower resp sx is a Wk longer which also fits with timing of sick cases we started seeing here, after we all assumed it was endemic as of late Jan/early Feb).
- based on our hospitalized cases (including the not formally diagnosed ones who are obviously COVID it is quite clinically unique) about 1/3 have mild lower resp sx, need 1-5L NC. 1/3 are sicker, FM or NRB. 1/3 tubed with ARDS.
- Thus far, everyone is seeing: nl WBC. Almost always lymphopenic, occasionally poly-predominant but with nl total WBC. Doesn't change, even 10days in. BAL lymphocytic despite blood lymphopenic (try not to bronch these pts; this data is from pre-testing time when several idiopathic ARDS cases) fevers, often high, poss intermittent; persistently febrile, often for >10d. It isn't the dexmed, it's the SARS2. low ProCalc; may be useful to check initially for later trend if concern for VAP etc. up AST/ALT, sometimes alk phos. 70-100 range. No fulminant hepatitis. Notably, in our small sample, higher transaminitis at admit (150-200) correlates with clinical deterioration and progression to ARDS. LFTs typically begin to bump in 2nd week of clinical course. mild AKI (Cr <2). Uncertain if direct viral effect, but notably SARS2 RNA fragments have been identified in liver, kidneys, heart, and blood.
- characteristic CXR always bilateral patchy or reticular infiltrates, sometimes perihilar despite nl EF and volume down at presentation. At time of presentation may be subtle, but always present, even in our pts on chronic high dose steroids. NO effusions.
- CT is as expected, rarely mild mediastinal LAD, occ small effusions late in course which might be related to volume status/cap leak. Not more helpful than CXR.
- when resp failure occurs, it is RAPID (likely 7-10d out from sx onset, but rapid progression from hospital admit). Common scenario for our pts is, admit 1L NC. Next 12hrs -> NPPV. Next 12-24hrs -> vent/proned/Flolan 18/ interestingly, despite some needing Flolan, the hypoxia is not as refractory as with H1N1. Quite different, and quite unique. Odd enough that you'd notice and say hmmm.
- thus far many are dying of cardiac arrest rather than inability to ventilate/oxygenate given the inevitable rapid progression to ETT once resp decompensation begins, we and other hosps, including Wuhan, are doing early intubation. Facemask is fine, but if needing HFNC or NPPV just tube them. will need a tube anyway, & no point risking the aerosols. no MOSF.
- cardiomyopathy. multiple pts here have had nl EF on formal Echo or POCUS at time of admit (or in a couple of cases EF 40ish, chronically). Also nl Tpn from ED. Then they get the horrible resp failure, sans sepsis or shock. Then they turn the corner, off Flolan, supined, vent weaning, looking good, never any pressor requirement. Then over 12hrs, newly cold, clamped, multiple-pressor shock that looks cardiogenic, EF 10% or less, then either VT->VF-> dead or PEA-> asystole in less than a day.
- Needless to say this is awful for families who had started to have hope. We have actually had more asystole than VT, other facilities report more VT/VF, but same time course, a few days or a week after admit, around the time they're turning the corner.
- Treatment - *Remdesivir might work, some hosps have seen improvement with it quite rapidly, marked improvement in 1-3 days. ARDS trajectory is impressive with it, pts improve much more rapidly than expected in usual ARDS. Recommended course is 10d, but due to scarcity all hosps have stopped it when pt clinically out of the woods - none have cont >5d. May cause LFT bump, but interestingly (200s-ish) for a day or 2 then rapidly back to normal suggests not a primary toxic hepatitis.
- unfortunately, the Gilead compassionate use and trial programs require AST/ALT <5x normal, which is pretty much almost no actual COVID pts. Also CrCl>30, which is fine. CDC is working with Gilead to get LFT reqs changed now that we know this is a mild viral hepatitis. currently the Gilead trial is wrapping up, NIH trial still enrolling, some new trial soon to begin can't remember where.
- steroids are up in the air. In China usual clinical practice for all ARDS is high dose methylpred. Thus, ALL of their pts have had high dose methylpred. Some question whether this practice increases mortality.
- it is likely that it increases seconday VAP/HAP. China had a high rate of drug resistant GNR HAP/VAP and fungal pna in these pts, with resulting increases mortality. We have seen none, even in the earlier pts who were vented for >10d before being bronched (don’t do now) 29/ - unclear whether VAP-prevention strategies are also different, but wouldn't think so? Hong Kong is currently running an uncontrolled trial of HC 100IV Q8. general consensus here (in US among docs who have cared for COVID pts) is that steroids will do more harm than good, unless needed for other indications. - many of our pts have COPD on ICS. After some observation & some clinical judgment, is to stop ICS if able, based on known data with other viral pneumonias and increased susceptibility to HAP. Thus far pts are tolerating that, no major issues with ventilating them that can't be managed with vent changes. We also have quite a few on AE-COPD/asthma doses of methylpred, so will be interesting to see how they do.
- "With the time and resources needed to go into the room of a patient getting ruled out for #COVID19, we try to think carefully and plan ahead before entering the room because we can’t go back and forth so easily." (Twitter @KiraNewmanMDPhD, 3/15/2020)
- (This report was retracted 3/15/2020 by @scott_mintzer "because of concerns about both the amount of attention is was getting and the accuracy of some of the information." A copy of the original account can be found here (Reddit).) "None are sleeping more than a couple hrs a night. Everyone is utterly exhausted. My colleague has seen so many people die as to have become totally numb.... there were no IV pumps available. So the nurse had given some of it, left the syringe attached, and planned to come by to give more a little later, and then finish it.... In short, this is a nightmare, teetering on the precipice of even worse destruction. The goal of every American city should be to avoid becoming the next Seattle." (Twitter @scott_mintzer, 3/15/2020)
- "Things are tough, he says, but not apocalyptic.... Radiology volumes are down because of cancellation of elective stuff. Radiology has capacity" (Twitter @RogueRad, 3/16/2020)
- "One of our UW Medicine hospitals just closed the OR to convert to ICU to manage COVID-19 cases." (Twitter @gorejohn 3/16/2020)
- "I’ve been surprised by the amount of fear not just from the public but also from other healthcare workers. I am becoming accustomed to caring for people with #COVID19, yet many are still not. It manifests as friction and pushback when calling a consult." (Twitter @KiraNewmanMDPhD 3/21/2020)
California
- "Tough week in hospital: More COVID-19 cases including my hospitalized colleague; a sick pregnant mom induced bc of COVID-19; all the usual death and badness from cancer, sepsis and CV disease. COVID-19 a marathon. Made the mistake of thinking a sprint." (Twitter @Shepinions 3/23/2020)
Michigan
- "6 out of my 18 patients all should have been tested for the coronavirus, and I could only test one of them.... Cannot test the patients I need to test" (Twitter @DrRobDavidson 3/18/2020)
New Jersey
- "So far I've treated 5 confirmed COVID-19 patients reqiring hospitalization, and currently have 14 suspected cases... and I can tell you that in 18 years of medical practice I've never seen anything like this" "It's a severe viral pneumonia. The problem is there is a flood of COVID-19 suspected cases coming to the ER, and we are quickly filling the hospital with them" (Twitter @BioBreakout, 3/14/2020)
- "NJ ER/ICU doc here. We are already overrun. And without appropriate cleaning/protective equipment." (Twitter @CHRISTO37877949, 3/14/2020)
- "What we’ve seen in the patients who ultimately are positive is that things can turn very rapidly. We had a patient that we were thinking about releasing — he seemingly was recovering — and then, two days later, he was put in the ICU. The flu isn’t like that.... Holy Name’s 11 positives are all males — and all between the ages of 28 and 48." (roi-nj, Life at the epicenter of N.J.’s coronavirus outbreak by Tom Bergeron 3/14/2020)
- "their hospitals are saying doctors & nurses will be *disciplined* for wearing protective gear, including masks." (Twitter @wendellpotter 3/21/2020)
Indiana
- "We're seeing some patients present to the ED with diarrhea, #COVID19 unsuspected but later confirmed" (Twitter @suzchongmd, 3/15/2020)
Misc
- "I am dead center in one of the hotspots. PPE is a HUGE problem.... I was offered one N95. Just one. No face shields... and those that have them are being told to wash them. No bunny suits.. just those flimsy yellow fabric gowns.... we will start dropping like flies very soon without proper safeguards in place" (Twitter @drjohnm 3/18/2020)
- "She has been seeing many patients & developed a cough. No fever. She asked if she should be tested. She was told no, more than once. She kept working, seeing patients, while using PPE. Now, she’s #COVID19 +" (Twitter @AshleySumrallMD 3/18/2020)
Patient/community experiences
| back to top |
China
- "A thread about what I observed in Chinese society, and what you should be mentally prepared for" (Twitter @tony_zy, 3/6/2020)
- "A regular person’s journey on Douban. In the past few weeks I’ve witnessed hundreds if not thousands of tragedies unfolding before my eyes" (Twitter @tony_zy, 2/8/2020)
United Kingdom
- "The anorexia is profound. It has taken 5kg off me, fortunately I can take that but I'm utterly knackered." (Twitter @Doctor_IMF, 3/16/2020)
- "Shivers and sweats were the story of the day. That and being utterly exhausted, with whole-body ache. Random temp: 38.5. One flight of stairs then stop for a rest. No appetite at all." (Twitter @GoughCJ, 3/16/2020)
- "D9: Feeling much better today. No headache. No cough. Exhaustion much improved. Appetite pretty much normal. I am 95% back to normal." (Twitter @GoughCJ, 3/19/2020)
- "Every swallow brings tears to your eyes, it’s just so painful.... I was surprised it completely poleaxed me. I could barely move from the sofa to the bed.” Dr. Ben Lovell as told to the Standard, 3/20/2020
- "post-Covid19 I have completely lost my sense of smell, and most of my sense of taste. It’s astonishing. My cup of tea tastes like hot water. Can’t smell my aftershave." (Twitter @DrBenLovell 3/23/2020)
United States
- "The last one week, it has been hell." (Twitter @pulte, 3/8/2020)
- Update: "“After I received the first dose, my fever went down and all the lab result is getting better,” Cai said. “I think those two medications slow down my virus. I took those two medications for four days and March 11 is the day I got the clinical trial medications. After that medication for one day, all my symptoms getting better. My oxygen level is not dropping anymore.” (3/16/2020 CBS New York)
- "My boyfriend and I have self-quarantined ourselves in our apartment since Feb. 23rd." (Twitter @microbeminded2, 3/9/2020)
- "Basically had a low grade fever for a few days then a bad cough, that turned into respiratory failure. I came in and they had to put me on high flow oxygen (3 times normal)...hence ICU.... I was the first COVID19 patient in the ICU on Thursday. Now there are many more." (Twitter @ClementYChow, 3/15/2020)
- "for those who get severe cases, like me, it’s been hell. I’ve had 10 days & counting, with no real improvement, of fever, fatigue, joint aches, chills, cough, respiratory difficulty. I have never been this sick in my entire life." (Twitter @DavidLat 3/17/2020)
- "Never in my life have I been this ill. “Young people aren’t at risk, they’ll only have mild symptoms” Wrong." (Twitter @bradleyziffer 3/19/2020)
- "I m a Cardiology fellow, NY, no PMH, fighting COVID infection 4 a week. Fevers, cough -> wheezing/SOB, on Hydroxychloroquine+Azithromycin, got worse on 2nd day of it, now in MICU. Got iv Tocilizumab, hoping to improve" (Twitter @jigneshpatelMD, 3/21/2020)
- "The resident did not have ANY of the classic symptoms of fever, cough or rhinorrhea. Instead, the resident had headache, muscle aches, sore throat, and chest tightness. The symptoms were all mild, vague, and could have been easily ignored. It is imperative that clinicians on the front line continue to be vigilant and advocate for expanded testing." (Twitter @davidhaomd, 3/21/2020)
Spain
- "Day 1 after #COVID diagnosis. Sore throat, headache (strong!), Dry cough but not shortness of breath." (Twitter @yaletung 3/9/2020). Day 2. Day 3. Day 4: "More cough & tiredness (very badly), still no dyspnea/chest pain." Day 5. Day 6. Day 7: "Cough & weakness got worse (again), still no dyspnea." Day 8: "Less Cough & similar weakness, still no dyspnea or red flag symptoms. No fever. SpO2 96%.... On paracetamol + HCQ." Day 9. Day 10. Day 11 "Less tired & cough, unable to endure small efforts." Day 12.
Testing
- YouTube video on how to collect a nasopharyngeal swab
- University of Washington Virology "Licensed medical practitioners from anywhere in the US can order #SARSCoV2 #CoronavirusUSA testing from @UWVirology. We continue to add capacity and can test hundreds more people daily." (Twitter @UWVirology 3/9/2020)
- FDA FAQs on Diagnostic Testing for SARS-CoV-2 - lists acceptable swab/media, that single swab may be adequate
- % of detection of SARS-CoV-2 in Different Types of Clinical Specimens, JAMA 3/11/2020
- Guidelines and patient criteria for COVID-19 testing by MA state public health vs. commercial laboratories 3/13/2020
- Drive-through testing experience in New Rochelle, NY: "There were big electronic signs saying KEEP WINDOWS CLOSED so we had to communicate through a closed car." (Twitter @sarahrosen 3/18/2020)
Hematology/Oncology meetings
| back to top |
An extensive list is available at The Cancer Letter website.
Canceled
- AMIA Informatics Summit (3/23/2020 to 3/26/2020, Houston, TX) - CANCELED
- SGO (Society of Gynecologic Oncology) 2020 Annual Meeting on Women’s Cancer, (3/28/2020 to 3/31/2020, Toronto, Canada) - CANCELED (may be rescheduled for in-person or virtual meeting)
- European Haemophilia Consortium (EHC) Youth Leadership Workshop (4/3/2020 to 4/5/2020, Amsterdam, Netherlands) and World Haemophilia Day (4/24/2020, Brussels, Belgium) - CANCELED
- ASCO Annual Meeting (5/29/2020 to 6/2/2020, Chicago, IL) - CANCELED
Postponed
- 1st Translational Research Conference: Chronic Lymphocytic Leukaemia (3/20/2020 to 3/22/2020, Paris, France) - POSTPONED until November 17-19, 2020
- NCCN Annual Conference (3/20/2020 to 3/22/2020, Orlando, FL) - POSTPONED until TBA
- Summit on National and Global Cancer Health Disparity (4/3/2020 to 4/4/200, Seattle, WA) - POSTPONED until Fall 2020
- AACR Annual Meeting (4/24/2020 to 4/29/2020, San Diego, CA) - POSTPONED until TBA
Rescheduled as virtual meeting
- ENETS Conference for the Diagnosis and Treatment of Neuroendocrine Tumor Disease - VIRTUAL MEETING
Still happening as planned
- None
General information
| back to top |
Trackers
- COVID-19 Coronavirus tracker for United States and Canada, with case-by-case descriptions (1point3acres.com)
- Johns Hopkins CSSE Worldwide Coronavirus Tracker
- United States COVID-19 state-by-test testing results - COVID tracking project (covidtracking.com)
- Australia COVID-19 tracker (covid19data.com.au)
Number of cases/epidemiology
- ArcGIS charts and maps about COVID-19 cases, with multiple options to break down by country
- Animated bar chart race of COVID-19 cases outside China from 1/27/2020 to 3/11/2020 (gohkokhan.com)
- COVID-19 cases per 10 million people
- Clusters of disease spread in South Korea, "Patient 31" (Reuters, 3/3/2020)
- Cases per country as of 3/12/2020
- Italy vs. United States number of cases offset graph through 3/13/2020
Misc information
- John Campbell Youtube Coronavirus videos
- CDC.gov COVID-19 Coronavirus information
- Estimate of mortality rate by age (Twitter @DorsaAmir, 3/7/2020)
- Influenza vs. COVID-19 mortality rate by age (Twitter @AshokKumarSheo8, 3/7/2020)
- Ars Technica summary of COVID-19 information (Arstechnica.com, 3/8/2020)
- Response to COVID-19 in Taiwan Big Data Analytics, New Technology, and Proactive Testing (JAMA 3/3/2020)
- Coronavirus: Why You Must Act Now (Medium, Tomas Pueyo, 3/10/2020)
- COVID-19 Update; 3/14/2020. A Message From Concerned Physicians by Howard Luks MD (Medium 3/14/2020)
- UCSF Expert panel discussion 3/10/2020, notes by Jordan Schlain MD
- Dermatologist's guide to COVID-19 handwashing (Twitter @RoxanaDaneshjou, 3/15/2020)
- COVID-19 presentation slides by Michael Lin MD/PhD PDF 3/13/2020 (Twitter @michaelzlin 3/14/2020)
- Fei Zhou et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 Mar 11. PubMed link to original article